-
News
Latest news
Explore the latest news from the UK's forestry and wood sector
-
Our story
Our story
Modern forestry and wood is the sustainable sector of the 21st century: producing a green material while improving the way we use our land. See how today's forests benefit the economy, the environment and our communities.
-
Join Us
Join Us
There are numerous exclusive benefits to becoming a Confor member, browse this section to find out more
-
Resources
Resources
Keep up to date with the latest event listings, see who's hiring or browse our library of publications
-
About us
This is Confor
The voice of the forestry and wood sector - find out who we are, what we do and how to get in touch
We are Confor:
Our aim is to support sustainable forestry and wood-using businesses through political engagement, market promotion and supporting our members' competitiveness.
The forest and timber story
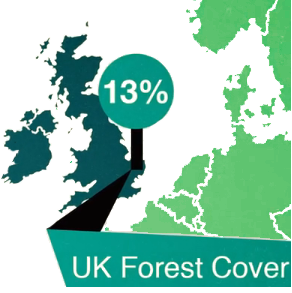
Forestry facts









 Events
Events

 Jobs
Jobs

 Forestry and Timber News
Forestry and Timber News
 Member Directory
Member Directory